
If you have been diagnosed with hepatic steatosis, don’t panic. It’s just another name for having a fatty liver.
As the name suggests, fatty liver means you have extra fat in your liver. This can make it difficult for the liver to function efficiently.
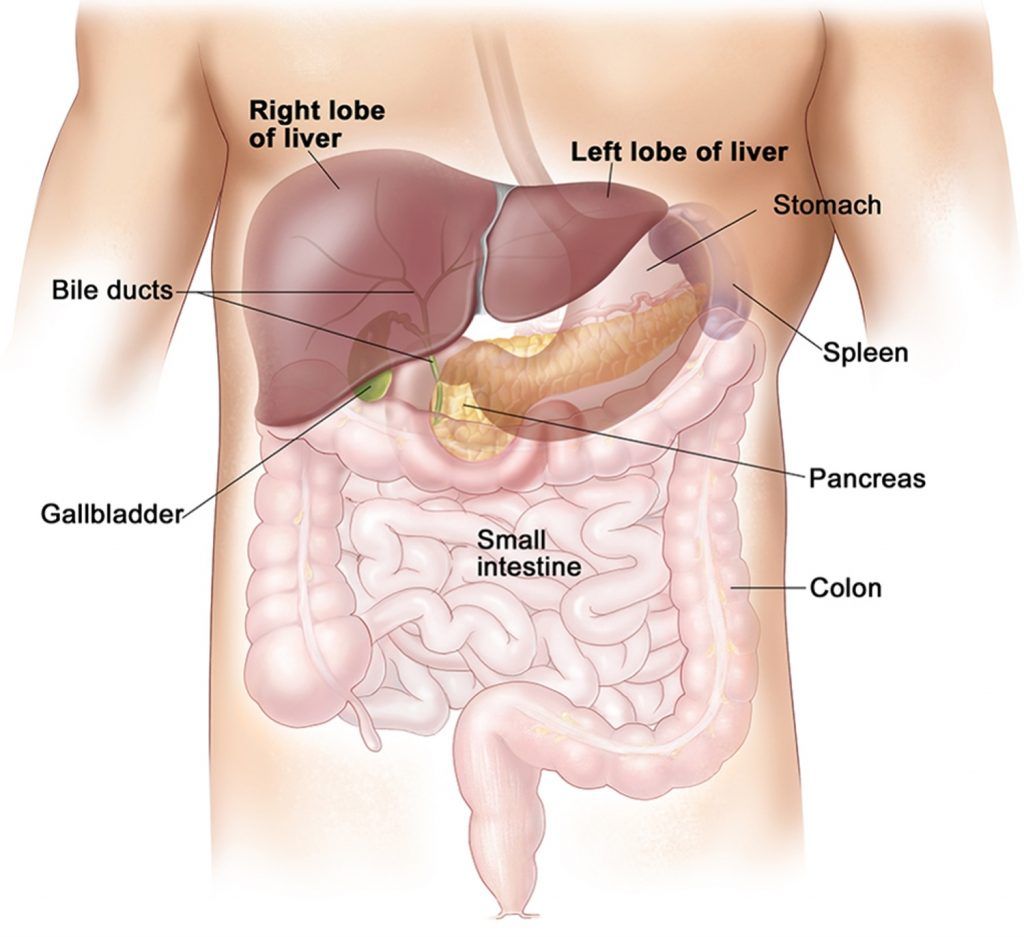
The liver is the largest internal organ in our body. It is located in the upper right part of the abdomen (1). The liver performs over 500 complex functions in the body. It is involved in digestion, nutrient storage, metabolism, immunity, detoxification, and many more essential processes in the body
Fatty liver is a very common health condition that affects millions of people around the world. In the early stages, it has almost no symptoms. But over time, as more fat builds up in it, the liver can get damaged. If not treated, this damage can worsen, eventually leading to more serious health complications.
But don’t worry. Fatty liver is easily reversible with the right treatment and lifestyle changes.
If you are at risk of developing fatty liver, you can even prevent it from occurring! But how do you even know if you are at risk? What causes fatty liver? How can I treat it? For all these answers and much more…keep reading!
Types and Stages of Fatty Liver Disease
Depending on its causes and stages, fatty liver disease is classified into two types, namely Non-Alcoholic Fatty Liver Disease (NAFLD) and Alcoholic Fatty Liver Disease (AFLD).
Non-Alcoholic Fatty Liver Disease (NAFLD)
You can get fatty liver even if you don’t drink any alcohol at all, or maybe just a drink once in a while. This condition is called non-alcoholic fatty liver disease.
Insulin resistance is the primary reason for most cases of nonalcoholic fatty liver disease. We’ll discuss this, in more detail, in the ‘causes of fatty liver’ section below.
Non-alcoholic fatty liver disease progresses through 4 stages of the disease:
Stage 1: Simple Nonalcoholic Fatty Liver
A little bit of fat in the liver is normal. But when more than 5 to 10% of the liver weight is due to fat accumulation, then you are said to have fatty liver (2). This is known as stage 1 fatty liver or simple fatty liver.
In this stage, there is no inflammation or other complications arising from having fatty liver. Many people remain unaware they have this condition since there are no obvious symptoms.
Stage 2: Non-Alcoholic Steatohepatitis (NASH)
This is a more severe form of nonalcoholic fatty liver. The liver becomes swollen and liver tissue becomes damaged.
This can also remain a silent disease with little or no symptoms. But some people may experience discomfort or pain in the area where the liver is situated.
Stage 3 of NAFLD: Fibrosis
In the damaged areas of the liver, scar tissue gets formed. This is known as fibrosis. At this stage, the liver still has enough healthy tissue to continue functioning.
Many people remain symptom-free even at this stage although fatigue or nausea are reported by some (read more about this in the ‘symptoms section’ of the article)
Treating the cause of your fatty liver at this point can help prevent the progression of your disease and even reverse some of the damage done (3).
Stage 4: Nonalcoholic Cirrhosis
If the fibrosis spreads to more damaged areas and extensive scar tissue replaces the healthy liver tissue, this results in liver cirrhosis.
The term cirrhosis comes from the Greek word ‘kirrhos’, meaning orange-colored and it refers to the orange-yellow appearance of the liver at this stage (4). The hard scar tissue can completely block liver function thus causing liver failure (5).
Alcoholic Fatty Liver Disease (AFLD)

Drinking small amounts of alcohol over a long period or binge drinking for a few days can cause fat to accumulate in the liver. This condition is called Alcoholic Fatty Liver (AFLD)
In its initial stages, stopping alcohol for just two weeks can reverse Alcoholic Fatty Liver, allowing your liver to start healing (6).
Alcohol-Related Liver Disease (ARLD) results from the damage caused to the liver by years of alcoholism (7). There are various stages of severity for ARLD. Alcoholic fatty liver disease is considered the first stage of ARLD. If not corrected, this can further develop into alcoholic hepatitis and/or alcoholic cirrhosis.
Alcoholic Steatohepatitis (ASH):
This is also known as alcoholic hepatitis. The fatty liver becomes swollen and inflamed. Symptoms of alcoholic hepatitis include fever, nausea, jaundice, etc.
Alcoholic Cirrhosis:
Cirrhosis is considered the end-stage of fatty liver disease. This results when the liver has become significantly scarred. The extensive scar tissue disrupts the functioning of the liver, eventually causing liver failure.
Functions of the Liver

Before moving on to the causes of fatty liver, you first need to have an idea of what the liver does. Then we can move on to how fat builds up in the liver, what causes fatty liver, and how to reverse this condition.
The primary functions of the liver include:
1. Filters toxins: Various harmful substances (toxins) enter the body through food, air, etc. These toxins are broken down into less harmful or harmless substances by the liver. The liver also filters out toxins from the blood that passes through it before allowing circulation to the rest of the body.
2. Stores nutrients: The liver stores fat-soluble vitamins A, D, E, K as well as the water-soluble vitamin B12. It also stocks up minerals like iron and copper. All these nutrients are released again into the blood when required by the body (8).
3. Produces bile: The liver produces a greenish-yellow viscous liquid called bile. Bile is produced by the liver round the clock and it oozes out through thin pipes called the bile ducts. Bile is used by the body to digest the fat we eat. The liver also pushes the toxins out through the bile. It mixes with the waste left over from the digestive process to form stool, which is passed out of your body.
4. Glycogen metabolism: Our body stores some amount of glucose, in our muscles and liver, in the form of glycogen. The liver converts excess carbohydrates to glycogen for storage. This process is called glycogenesis. Glycogen acts as a fuel reserve. Glycogen can be easily broken down, to make glucose, when required by the body. This process is called glycogenolysis. It helps maintain blood sugar levels (9).
5. Fat metabolism: With the help of insulin, excess carbohydrates and proteins are converted into fatty acids and triglycerides (10). This process is called lipolysis. The triglycerides get stored as body fat (11).
6. Produces cholesterol: Your liver produces about 80% of the cholesterol you need for the healthy functioning of your body. The remaining 20% comes from your diet (x). Cholesterol has many important roles in your body. It is needed for the synthesis of vitamin D and for the production of hormones such as testosterone and estrogen. The liver also excretes excess cholesterol into the bile (12).
7. Blood clotting factors: With the help of vitamin K, the liver makes the proteins needed for blood clotting (13).
Development of Fatty Liver
Now that you have an idea of what the liver does, let’s try to understand how fatty liver develops.
Fat can build up in our body due to two primary reasons:
- Your body produces too much fat due to excess intake of energy.
- Your body cannot metabolize fat efficiently due to impaired gut health, infection, or inflammation (14).
Energy sources in our body: The energy from the foods we eat comes from the carbohydrates, proteins, and fats in our diet. Carbohydrates are broken down into glucose (blood sugar). Protein is broken down into amino acids for the body’s use and excess amounts of it in the diet are converted to glucose (15). Fats break down to form fatty acids. Both glucose and fatty acids are energy sources (the fuel) for our body’s functions.
How excess energy is stored: Once the glycogen stores are full, the liver converts excess glucose to triglycerides. Extra fatty acids are also converted to triglycerides (16). These triglycerides are stored in our fat cells as an energy reserve. These fat stores are just below your skin. They are known as subcutaneous fat.
Fatty infiltration of the liver: Once these fat cells under the skin are full, the leftover energy gets stored in and around various organs in our body. This is known as visceral fat. It is found inside the abdominal cavity and wrapped around your intestines and other internal organs such as the liver, pancreas, and kidneys (17).
Insulin resistance is the mechanism behind this occurrence. So let’s try to understand how this happens.
Causes of Fatty Liver
As mentioned earlier, insulin resistance is the primary cause of non-alcoholic fatty liver disease.
The hormone insulin is produced by the pancreas. When energy-giving glucose is released into the bloodstream, insulin notifies your body cells to accept this fuel. But if these cells are already filled to capacity, they reject insulin’s request. Your pancreas reacts to this resistance by increasing insulin production. Overwhelmed by the rising insulin levels, cells stuff themselves till they can take no more.
This condition is called insulin resistance, the truth is that it’s impossible for the cells to accept any more. This results in high levels of glucose in your blood. The liver converts the excess glucose (and excess fatty acids) to triglycerides for fat storage.
But since the fat storage cells have no room left, all this gets deposited as visceral fat over your internal organs. Thus insulin resistance can lead to non-alcoholic fatty liver.
Some people may get a fatty liver during pregnancy.
Acute fatty liver of pregnancy (AFLP): This is a rare pregnancy complication that causes acute fatty liver. It is seen in the third trimester. This type of fatty liver disease creates serious risks for both the mother and her baby (18). Once diagnosed, your doctor will attempt to deliver the baby at the earliest. This takes the stress off your liver and enables it to heal and return to normal within a few weeks after delivery.
What are the Symptoms of Fatty Liver Disease?
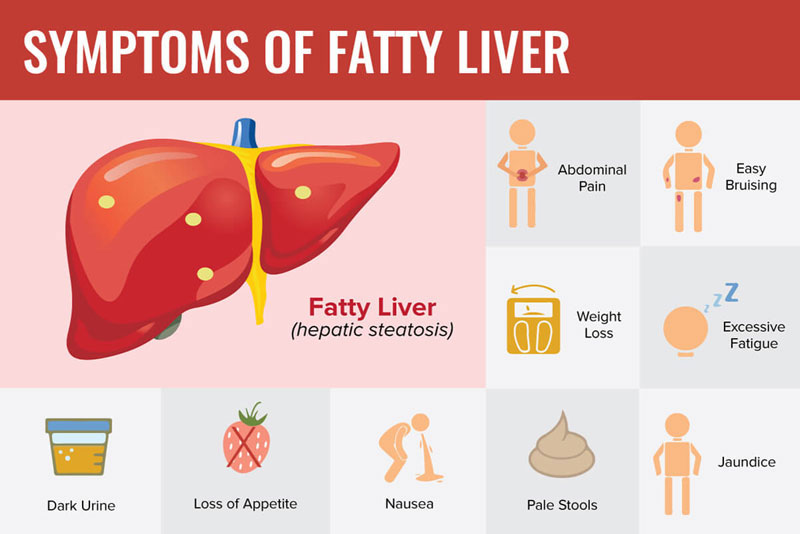
Fatty liver disease tends to be free of symptoms for most people, especially in the initial stages. You may experience sugar cravings, hunger, weight gain, and sluggishness. As the disease progresses, symptoms such as fatigue and nausea may be experienced by a few people.
Fatty liver can cause the liver to get enlarged (hepatomegaly). Again, most people may not be aware they have this. But some people may experience a feeling of fullness in that area of their body where the liver is located. Pain in the upper right abdomen and in the right shoulder blade is also reported as a symptom.
The symptoms of ASH (alcoholic steatohepatitis) or alcoholic hepatitis include fever and nausea. If their eyes and skin have a yellowish color – this indicates jaundice. Their liver may be inflamed and enlarged (19).
At the stage of NASH and finally liver cirrhosis, symptoms may become more evident. Other than the above-mentioned signs and symptoms, those with this condition may experience:
- Physical weakness
- Extreme tiredness
- Loss of appetite
- Mental confusion
- Itchy skin
- Nose bleeds
- Bruising easily
- Severe muscle cramps
- Swelling of legs
- Jaundice (yellowing of skin and eyes)
- Spider-like blood vessels
- Redness of palms
- Gynecomastia (breast enlargement in men)
- Caput medusae (network of dilated veins surrounding the umbilicus)
- Ascites (fluid accumulation in the abdomen)
- Petechiae (small red spots caused by bleeding into the skin)
- Enlarged spleen
How is Fatty Liver Disease Diagnosed?
Considering its lack of obvious symptoms, a fatty liver is more often spotted during an abdominal ultrasound or blood test for other medical conditions.
Medical history: The doctors will need to know your diet and alcohol consumption habits to identify if you have ALD or NAFLD. They will need information on your personal medical history and the medications you have been taking. They will also ask for your family history, especially regarding liver-related diseases and metabolic disorders. You should explain if you have been experiencing symptoms such as fatigue, nausea, loss of appetite, etc.
Physical examination: The doctor may check to see if he can feel any liver enlargement. But in many cases, the liver may not be enlarged even if inflammation is present.
Blood tests: Your doctor may note elevated liver enzymes in a routine blood test and recommend running more tests. SGPT & SGOT are the enzymes produced by the liver. High levels of these enzymes indicate liver cell injury. Lipid profile, fasting insulin, and blood glucose levels should also be noted during blood tests. A liver function test with GGT may be suggested as the enzyme Gamma-glutamyl Transferase (GGT) may leak into the bloodstream if the liver is damaged.
Imaging studies: Ultrasound scans, CT scans, and MRI scans are imaging tests used for confirming a fatty liver diagnosis.
FibroScan®: Vibration-controlled transient elastography (VCTE) is a specialized ultrasound that helps measure the amount of fat and scar tissue in the liver.
Liver biopsy: A liver biopsy is conducted only if you are at risk for NASH complications and cirrhosis. It is also used for differentiating between NAFL and NASH. This is not routinely done or used for diagnosing simple fatty liver disease.
A small piece of liver tissue is removed for examination by inserting a needle into the liver. You may experience only mild discomfort during the procedure due to the local anesthetic provided. Examining the liver tissue is the best way to confirm how far the liver disease has progressed and the extent of fibrosis or scarring.
How is Fatty Liver Disease Treated?
There are no medications for treating a non-alcoholic fatty liver. But don’t worry, you don’t need any medication to correct this condition.
The treatment for non-alcoholic fatty liver is as simple as losing weight. Considering that the accumulation of fat on the liver happens due to a lack of space in the fat cells, the solution is as simple as emptying those cells and making space available.
But what if I am already slim, but I have been diagnosed with a fatty liver?
Well, you still have to lose weight and get your body fat below your personal fat threshold (PFT).
What is Personal Fat Threshold (PFT)?
The excess fat in our body is supposed to be stored as subcutaneous fat. This is the fat under our skin – on our arms, thighs, hips, buttocks, chest, etc. As subcutaneous fat increases, it makes us look fat.
We all have different capacities to store this subcutaneous fat. This is known as your personal fat threshold or PFT (20). There is a set limit or a threshold to your personal capacity to store fat.
Once you reach your own personal fat threshold, your subcutaneous storage capacity reaches its maximum. Now your body is forced to store the fat elsewhere. So, the fat starts accumulating in and around internal organs. This visceral fat – which we can’t see- is dangerous to our health as it is the beginning of fatty liver and all metabolic syndrome diseases.
All of us have different personal fat thresholds. A person with a high PFT can become quite fat before visceral fat builds up. On the other hand, a slim-looking person may have a fatty liver because they have low PFT.
So even if you are a slim person, you can reverse fatty liver disease if you bring your body fat levels below your personal fat thresholds (PFT levels).
Diet for Treating Fatty Liver:

So, what’s the best diet for fatty liver and weight loss?
- Foods to add:
- To keep the damages to the liver low: Cruciferous vegetables, beet, and carrot. These help the liver work better.
- To avoid reactive hypoglycemia: Low carb, moderate protein, and high-fat foods
- Foods to avoid:
- To avoid reactive hypoglycemia: Sugary fruits, sugary drinks and foods, and other refined carbohydrates
- To lose weight and reverse fatty liver: All (partly or fully)
You need to cut down on all refined carbohydrates and added sugar to your diet. Follow a low carbohydrate diet with moderate amounts of protein and healthy fats. Have plenty of fresh vegetables, especially leafy greens and cruciferous vegetables. It may be best to limit your intake of fruits such as mangoes and grapes till you have lost a considerable amount of weight. Eggs, chicken, beef, mutton, and seafood are great additions to a healthy diet.
Treatment for Alcoholic Fatty Liver: This is also quite simple, but not so easy to execute. First, you need to stop drinking alcohol. You also need to bring your body fat below your PFT levels.
Alternative Treatments for Fatty Liver: Most of us prefer finding natural ways to cure fatty liver. While looking to reverse fatty liver, we come across homeopathic medicines for fatty liver and fatty liver ayurvedic medicines. The evidence of these treatments is mostly anecdotal. However, we do know that losing body fat and bringing it under your PFT is a natural cure and the best way to reverse fatty liver.
The Downstream: Is Fatty Liver Dangerous?
If I have a simple fatty liver with no symptoms, then what’s the big deal? Do I really need to reduce my body weight and bring it under my PFT levels? Are there any dangers to having a fatty liver? Why should I try to reverse the fatty liver?
If you have a fatty liver, then you also have insulin resistance (as explained in the causes of fatty liver).
If not corrected, this can lead to type-2 diabetes, high cholesterol, and hypertension. You can end up with metabolic syndrome where you have all these three metabolic disorders. This increases your risk of heart disease and stroke.
In women, Polycystic Ovary Disease (PCOD) is also caused by insulin resistance. The high insulin levels can cause the ovaries to overproduce testosterone (21, 22). As the testosterone-estrogen hormone balance is disrupted, PCOS symptoms can emerge. This includes cysts in the ovaries, facial hair growth, male pattern baldness, acne, etc.
Then, there is always the danger of fatty liver disease progressing to its next stages of NASH, fibrosis, and cirrhosis. Liver failure can result from cirrhosis, and this can be life-threatening. You may need a liver transplant at this stage. Having cirrhosis also increases the risk of liver cancer.
Conclusion
The primary cause of non-alcoholic fatty liver is having a body fat level above your personal threshold level. To reverse your fatty liver disease, you must reduce your weight and bring it under your PFT levels.
