
Are you suffering from a chronic cough for no apparent cause? Do you feel a lump in your throat? Does it feel hoarse? LPR or Laryngopharyngeal Reflux could be the cause of your woes.
As the name Laryngopharyngeal Reflux suggests, the affected areas are mostly your larynx (the voice box) and the pharynx (the part of the throat behind the mouth).
Although symptoms can be noted in some people, it’s not so evident in others. So, this condition is often termed Silent Reflux.
But LPR can cause damage to the esophagus, throat, vocal cords, and even the nasal passages. Many people remain unaware of their condition till more serious symptoms arise due to stomach acid damage.
Diet and lifestyle changes go a long way in treating LPR. Medications and sometimes surgery may be required in some cases. A proper assessment of when to eat and what to eat can help ease most of your discomforts.
What is Laryngopharyngeal Reflux (LPR)?
To understand how LPR occurs, you first need to understand what is acid reflux.
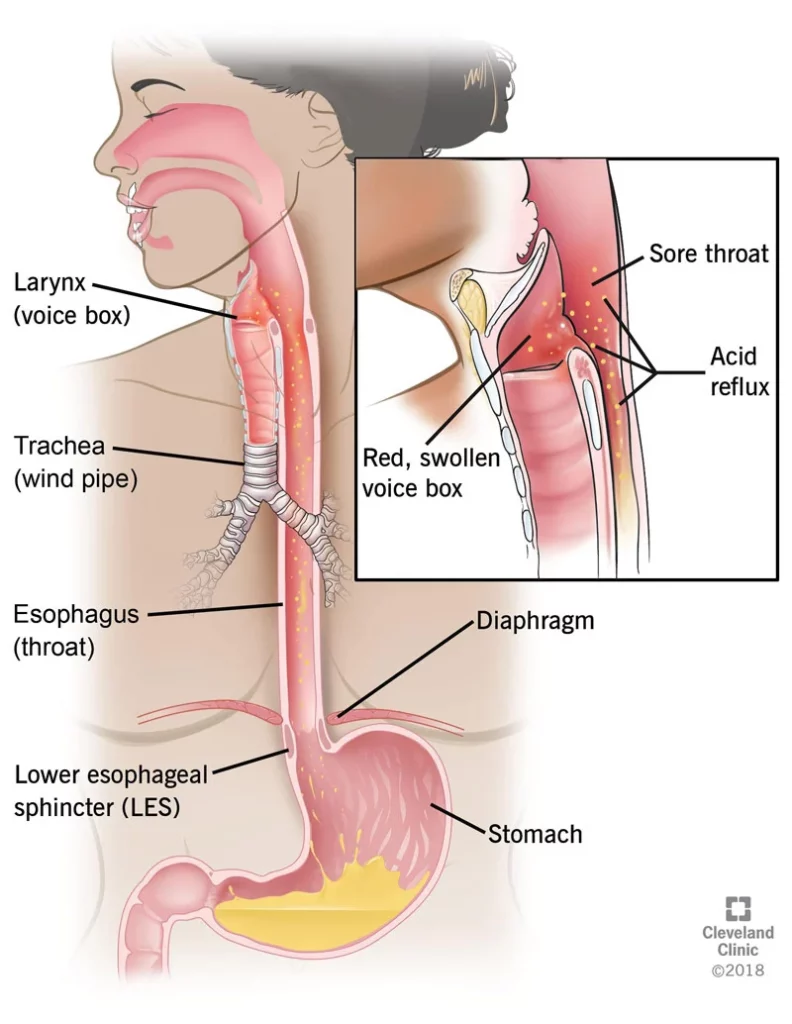
Acid reflux occurs when your stomach acid flows back up into your esophagus (food pipe). This causes irritation and inflammation of the esophageal lining. This is often experienced as heartburn or discomfort in the chest area.
The lower esophageal sphincter (LES) controls the opening between the stomach and your esophagus. Usually, this door remains closed except for the time you eat and the food has to pass down to the stomach. When the sphincter muscle fails to close this door properly, the stomach acids may get pushed back up into the food pipe.
However, when this acidic stomach content flows further toward your throat, larynx (voice box), and even nasal passage, the condition is called Laryngopharyngeal reflux (LPR) (1).
LPR can lead to complications related to your sinuses, middle ear, throat, vocal cords, and even lungs. Several respiratory symptoms such as cough, wheezing, feeling a lump in the throat, chronic throat clearing, etc are often associated with LPR.
Who is More Prone to Laryngopharyngeal Reflux?
Laryngopharyngeal reflux (LPR) can happen to anyone. This condition can be seen in babies as young as a few weeks old. However, people of any age and sex can develop this silent reflux.
LPR in Infants: LPR is commonly seen among infants and younger children (2). The esophageal sphincter muscles, which prevent the stomach content from flowing back towards the food pipe, are underdeveloped at birth. This makes the babies more prone to refluxes (3). Their liquid diet and constantly lying down are contributory factors as well.
LPR in Children: As the infant grows older and the esophageal sphincter muscles strengthen, refluxes tend to stop. But if they are weak or relaxed, the stomach contents can flow back up into the throat. Several factors can lead to this condition such as hiatal hernia, certain medications, secondhand smoke, some previous surgery, or a developmental delay. Obesity is also believed to be one of the major contributory factors of LPR in children (4), (5).
LPR in Adults: LPR in adults often exhibits very few symptoms. They may experience heartburn or chest discomfort, a burning sensation in their throat, or a bitter taste at the back of their throat. Hoarseness and persistent cough are other common symptoms. Chronic stress, excess weight, and unhealthy dietary habits increase the risk of LPR.
What Causes Laryngopharyngeal Reflux (LPR)?
Several factors lead to a condition where LES fails to close properly leading to the reflux of acid-containing contents back to the esophagus and upwards until the mouth. There are times when this acid even gets aspirated into the windpipe and lungs causing severe complications (6).
The factors that can cause LPR are:
- Obesity: Obesity is one major factor that can lead to increased intra-abdominal pressure leading to stomach acid leakage or backflow (7). Obesity can lead to a hiatal hernia that results in the development of backflow of acid.
- Esophageal valve damage: Several factors can lead to the damage or weakening of the esophageal valves. Under this condition, the valve is unable to prevent stomach acid from flowing back to the food pipe (8).
- Low amount of gastrin: Gastrin is a hormone that stimulates the production of gastric juice by the stomach. The lower amount of gastrin due to nutrient deficiency can result in lower gastric acid which is inefficient to keep the LES closed resulting in LPR.
- Poorly functioning Lower-Esophageal Sphincter (LOS): This condition is often associated with a hiatus hernia that can’t stop the gastric content from flowing back to the throat. It can either be liquid or gaseous, resulting in irritation or a nervous reflex such as a cough.
- Gastroparesis: This is a condition that is characterized by poor gastric emptying because of poor stomach nerves or weak muscular activity. If and when the stomach doesn’t empty properly because of poor motility or any other blockage, the pressure inside the stomach exceeds the LOS pressure causing reflux.
- SIBO (Small Intestine Bacterial Overgrowth): The good friendly bacteria that are present in our body usually reside in the large intestine. All the fermentation of food takes place there. Nutrients produced are absorbed and the remaining waste is ejected out.
In SIBO, there is an abnormal growth of bacteria in the small intestine. As a result, these microbes start fermenting carbohydrates there which, in turn, produces excess gas. This extra gas needs an outlet and tries to escape through the GI tract in the form of burping and belching leading to gaseous reflux to the throat.
- Low Stomach acid: The pH of the stomach acid is between 1.5 to 3.5 which is highly acidic. When the acidity in the stomach reduces and the stomach content is not acidic enough, the LES can’t close properly leading to LPR.
- Esophageal Inlet patch: In some people with LPR, it has been found that a small patch of acid-secreting tissue at the top of the esophagus can cause irritation to the adjacent larynx and pharynx. Some researchers believe it can be an embryological remnant.
- Upper esophageal sphincter (UOS) dysfunction: When you have a failing LOS, the valve at the top of the esophagus can become overactive in an attempt to protect the airways. Though its role in LPR remains unclear, the LPR symptom such as globus can be because of this.
What are the Symptoms of LPR?
The signs and symptoms of LPR are mostly experienced in the throat and chest (9), (10), (11).
These include:
- Hoarseness or voice problem
- The feeling of a lump or globus in the throat
- Need to clear the throat often because of the sensation of mucus stuck in the throat
- Bitter taste in your throat
- Soreness in the throat
- Difficulty in swallowing solids, fluids, or tablets also known as dysphagia
- Coughing after eating or lying down
- Ear pain
- Choking episodes
- Chest tightness
- Heartburn, chest pain, and indigestion
- Red, swollen, or irritated larynx
- Chronic cough
How Severe can LPR be?
Approximately 10 percent of the US population gets affected by LPR. In fact, around 50 percent of people with voice disorders are detected with silent reflux.
LPR can cause severe health problems if left untreated. They may lead to:
- noisy breathing
- lung disorders
- related breathing problems such as asthma and bronchitis
- choking episodes
- recurrent pneumonia
- oral cavity disorders persistent or repeated laryngitis/ laryngopharyngitis
If this continues, silent reflux can damage your throat and voice box completely. LPR can increase the risk of cancer in the area that is directly affected, such as the esophagus, lungs, throat, and larynx. However, for cancer to develop, LPR has to go undetected and untreated for years.
How can you Diagnose Laryngopharyngeal Reflux?
LPR diagnosis is mainly based on the patient’s symptoms (12). In some cases, testing is not needed while others need them.
The commonly used tests for LPR are:
- A Swallowing study: In this study, the patient has to swallow a special liquid called barium. This liquid forms a layer on the esophagus, stomach, and intestines and makes it easily outlined on an X-ray. The doctor then investigates the movement of food while it passes from the mouth to the esophagus.
- A clinical examination with a laryngoscope: The laryngoscope is used for the diagnosis of silent reflux by checking on the signs of laryngeal irritation and inflammation (13). The investigator examines and identifies edema and erythema, particularly in the posterior region of the throat.
- Endoscopy: The doctor can investigate LPR through an endoscope, which is a long thin tube with a camera fitted at the end. This is passed through the mouth, down the esophagus, and into the stomach (14).
- Esophageal pH test: This test measures and records the pH of the amount of acid that backflows into the esophagus. A thin, small tube with a device on the tip that can sense acid is passed via the nose, down to the esophagus, and positioned about 2 inches above the LES. With tape, the tube is fastened to the side of the face. It is fitted so that the end of the tube comes out of the nose. This part is attached to a portable recorder with several buttons that the patients can press to mark certain events (15).
- Intolerance Breath Test: In case the condition has occurred because of SIBO, malabsorption of sugars such as lactose or fructose and their fermentation will lead to bad breath. This test is done by giving the patient a sugar solution to drink and the exhaled breath is tested after two hours. The measurement of hydrogen and methane gases by gut bacteria confirms the same (16).
Treatment for Laryngopharyngeal Reflux (LPR)
LPR can be treated by making changes in your lifestyle and diet. It may also need the usage of medications and in some cases surgery. Let’s have a look at them individually.
Diet
- Weight Management: All kinds of reflux symptoms worsen with weight. A diet designed to reduce weight can help tackle LPR symptoms in obese people.
- Food Modification: Avoid fatty, spicy, and high acid-level foods. Do not take alcohol, tobacco, or caffeine.
- Low FODMAP for SIBO: If SIBO is the cause of LPR, then a low FODMAP diet can be advised to solve the problem. FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols.
These are short-chain carbohydrates and sugar alcohols that are poorly digested in the body, resulting in fermentation and releasing of gas. Low FODMAP in combination with a good antibiotic can improve your SIBO. Taking probiotics for the large intestine and medicines for improving gastrointestinal motility can successfully lead to better gut health.
- Consuming Potassium and Vitamin D: Potassium and vitamin D supplements can help reduce the incidence of LPR because of their role in the contraction of smooth muscles and the production of gastric acid-producing gastrin hormone (16), (17).
- Pepsin: Pepsin is an enzyme that digests protein. However, it has been shown to impair the constitution of the cell membranes and initiate inflammatory changes within the larynx, nasopharynx, and nasal cavity. Deactivating or neutralizing it can help. In fact, alkaline water has been known to deactivate pepsin.
- Low Residue: If gastroparesis is the reason for LPR, then a diet consisting of low fiber can help solve the issue.
Medication
In patients with LPR, acid isn’t always the problem. The main factor is the weakening of the valve which is unable to prevent reflux. However, in order to safeguard your body from the acidity of reflux, medicines are given. These medications usually make the liquid less acidic. They are:
- Proton Pump Inhibitors (PPIs): Proton pump inhibitors are medicines that reduce the production of stomach acid. They are believed to be highly effective for LPR. However, a high dose of medication for a prolonged period of time works well (18).
- H2 Blockers: H2 stands for histamines, a chemical that signals the stomach to produce acid. H2 blockers are medications doing the opposite, reducing the acid content of the refluxed material (19).
- Gaviscon Advance: Gaviscone advance is a form of alginate that forms a raft over the stomach contents so that if anything spills back into your esophagus or throat, it is less damaging (20).
- Ziverel: Ziverel can coat the esophagus with a soothing coat and can also help repair its lining. However, it is still undergoing evaluation to confirm its efficiency in LPR (21).
- Prokinetics agents: These medications increase gastric motility. It stimulates the forward movement of the GI tract and increases the pressure of the LOS. However, they aren’t used very often in long term because of their adverse effects.
- Antacids: These medications help neutralize the acidity of the stomach providing temporary relief to common symptoms such as heartburn (22).
- Sucralfate: These medicines protect the injured mucus membrane. They are anti-ulcer drugs used to treat ulcers of the upper GI tract and peptic ulcers (23).
If the condition is severe, surgery might be recommended for treatment.
Intervention
- LINX: LINX is a device consisting of a small band of titanium beads with magnetic cores connected together with titanium wires to form a ring shape. It is surgically implanted around the lower part of the esophagus and is used to treat reflux problems such as GERD and LPR.
- Fundoplication: It’s a kind of surgery in which the upper part of the stomach is wrapped around the lower esophagus and stomach. It can be done by laparoscopy. Fundoplication can also be done with proper surgery.
- Stretta: Stretta is not exactly a surgery. In this procedure, the gastroenterologist sends painless needles to the junction where the stomach meets the esophagus. These muscles are weak in patients with LPR. Through the needles, radiofrequency waves are sent into the muscle tissue which helps stimulate the growth of new cells. As these muscles or sphincters start gaining strength, the LPR issues start solving eventually.
- Pyloric dilatation: The pyloric sphincter is at the juncture of the stomach and intestine. It controls the speed of the food entering the intestine from the stomach. Often, in people, this sphincter is too tight and can cause delayed gastric emptying or LPR or acid reflux (GERD), as it forces the LES to open. Dilation of the pyloric sphincter with a balloon through an endoscope can help people permanently.
How Does Food Affect LPR?
Food plays a very important part in LPR. Choosing the right one for you can inevitably provide comfort.
Let’s take a quick look at the foods that can be extremely beneficial and reduce your symptoms while foods that when avoided can help you deal with LPR.
Foods That Can Help LPR
These foods can help you from the discomfort of reflux and can keep acid reflux at bay. They are:
- Bananas: They help the irritated and inflamed esophagus preventing discomfort from stomach acids. Consume half a banana 30 minutes before a meal and prevent heartburn.
- Ginger: They are a natural stomach soother with anti-inflammatory properties. It helps reduce inflammation of the esophagus, relieving painful reflux. It can also reduce nausea and alleviate indigestion.
- Turmeric: Like ginger, turmeric also has anti-inflammatory properties that can calm painful inflammation of the esophagus. It also increases gastric mucus which prevents the lining of the stomach wall from erosion and ulcers.
- Pineapple: Although this fruit is acidic, it actually helps relieve painful heartburn. Pineapple contains bromelain which has powerful antacid properties. They are high in fiber and water content that boosts digestion.
- Apples: Studies have claimed that one slice of apple can actually calm down acid production. It also reduces the burning sensation. They have the ability to neutralize the stomach in under 5 minutes.
- Almonds: They are a powerhouse of healthy fats that can relieve painful heartburn. They also contain enzymes that improve digestion preventing stomach acids from rising back up into the esophagus. The skin of almonds can reduce gastric acidity protecting the stomach wall from erosion. Also, the calcium in raw almonds can balance your acid level.
- Grapes: They can help relieve discomfort in an instant. Grapes promote digestion and soothe the stomach by neutralizing stomach acid.
- Buttermilk: If you drink half a cup of cold buttermilk, it may alleviate painful heartburn symptoms. The effects are quick and long-lasting. The buttermilk can prevent the lower esophageal sphincter from opening up and allowing stomach acid to rise.
- Chamomile tea: It is not just relaxing but also may relieve an inflamed or irritated esophagus. It helps to settle the stomach and prevent acid from backing up and causing discomfort.
- Apple Cider Vinegar: Just 2 tablespoons in half a cup of warm water will relieve heartburn by helping in the complete closure of the sphincter preventing reflux. It can calm the stomach, reduce esophageal inflammation, and promotes healthy digestion. Acidic food such as sauerkraut and pickles do the same.
- Cumin seeds: these seeds can calm the irritated nerves of the stomach and promote the healing of ulcers. The digestion gets a boost and eliminates gas. Put half a teaspoon of cumin seeds in half a glass of warm water after your meals and have it. You can also add half a teaspoon of cumin seeds to 1 liter of water and simmer it for 10 minutes.
Foods to Avoid for LPR
There are two categories of food that exaggerate the symptoms of LPR. It’s always a question of what you eat and when you eat.
The first group of food loosens the lower esophageal muscles. As the acidic stomach sits right underneath it, these 6 foods relax the muscle that separates the acidic stomach from the non-acidic esophagus.
They are:
- Caffeine
- Alcohol
- Chocolate
- Mint
- Raw onion
- Raw garlic
Coffee and chocolates also increase stomach acid proving to be a double whammy in the case of LPR.
The second group of food increases acidity in your stomach and as a result, helps activate the hormone pepsin in the body. They are:
- Sugary carbonated drinks such as colas and Pepsi
- Sugary drinks such as bottled iced tea
- Citrus
- Tomato sauce
- Vinegar
- Wine
Healthy Habits
In addition to that, practice these habits that can avoid situations that aggravate LPR problems:
- Avoid stress
- Stop smoking
- Avoid eating canned foods
- Have plenty of fluids
- Waiting at least 2-3 hours to lie down after eating
- Don’t overeat. Reflux occurs when your stomach is distended.
- Do not bend over or exercise after eating
- Eat smaller meals
- Chew well
Natural Remedies for LPR
For Infants and Children
Even though most infants outgrow this condition, a smaller percentage may still require treatment. Practicing certain habits can help your child. They are:
- Keeping the infant in an upright position for 30 minutes at least after feeding.
- Feeding your child smaller and more frequent meals rather than a big ones.
- Raise the head of your bed before sleeping. As the head and the upper portion of your child’s body are propped up, you can prevent the reflux of stomach acid.
For Adults
Apart from the changes in food and lifestyle which have been mentioned earlier, adults can benefit from these natural remedies. They are:
- Wearing loose clothing rather than body fitting or tight clothes.
- Change the way you sleep. Raising the head of the bed so that gravity helps prevent reflux. Placing foam pillows under the mattress can help you create a raised edge at the desired height.
- Bend your knees when picking up objects. This reduces pressure on your stomach.
- Monitoring what you eat will help you understand what triggers symptoms. What you eat, how much you eat, and when you eat are all factors that contribute to improving or worsening your condition.
Lifestyle changes and proper communication with your doctor can help you deal with this condition correctly.
Home Remedies for LPR
The acid from the stomach causes irritation, inflammation, and scarring which can tighten the esophagus, making it even more irritated. LPR is more common in overweight people because of the pressure on the esophagus.
We can’t undo things that are done. But some simple changes in life can definitely alleviate the LPR symptoms.
- If you are overweight reduce your weight to a healthy range
- Drink two ounces of unprocessed aloe vera juice a day
- Wait at least an hour after a meal before exercising
- A tablespoon of baking soda in half a cup of warm water can provide you with instant relief
- Don’t wear tight clothes as they add pressure
- Supplement with Saccharomyces boulardii, a probiotic strain specifically for the small intestine to help optimize absorption of key vitamins that maximizes digestive health
- Start the day with a cup of warm water with a dash of freshly squeezed lemon juice. This will enable your body to balance the acid levels in the stomach before introducing any food resulting in better digestion.
- Chewing gums can lead to greater saliva production that can reduce esophageal acid levels
- Slippery elm is effective in soothing sore throats. It also calms irritation in the digestive tract. This herb is available in different forms such as lozenge, capsule, or powder. Choose in accordance with your preference.
- Quit smoking
- Make sure to finish eating three hours before your bedtime. This will assure enough time for digestion. Don’t lie down directly after eating
- You must try sleeping with the head of your bed raised. Sleeping on your left side can also be beneficial. This is because the esophagus comes into the top of the stomach on the right side and lying on your left relieves the pressure
Frequently Asked Questions (FAQs) on Laryngopharyngeal Reflux (LPR)
1. What is the difference between LPR and GERD?
Laryngopharyngeal reflux (LPR) and Gastroesophageal reflux disease (GERD) are both the result of gastric reflux in areas that can’t tolerate this acid. The main reason is the weakening of the lower esophageal sphincter which normally acts as a gatekeeper and prevents this.
However, they are different (24). In GERD, the stomach acid flows back into the esophagus causing irritation in its lining and resulting in heartburn and acid indigestion. In comparison, in LPR, the stomach acid flows back into the larynx, pharynx, and even the nasal cavity.
This causes respiratory symptoms such as cough, wheezing, and a feeling of globus in the throat. It also results in inflammation of the sinus, pharynx, and the areas that face so. LPR may cause heartburn in some cases.
2. Can LPR be sent to permanent remission?
LPR might not be sent into permanent remission but the right treatment can help you recover completely for months or years. Most people with LPR need treatment from time to time and may have to continue with their medicine.
In advanced cases, surgery can offer relief for several years. However, effective medicine, lifestyle changes, and diet can definitely help reverse the situation.
3. Is spontaneous remission possible with LPR?
It has been noted that 25 percent of LPR patients experience spontaneous resolution of symptoms (25). However, about 50 percent of LPR patients continue having chronic symptoms with intermittent periods of remission and exacerbations.
4. Is there voice therapy for LPR?
Studies have noted that practicing voice therapy in addition to taking medication shows a greater degree of improvement in LPR patients. In addition to improvement in the hoarseness, breathiness, and jitter experienced by those with LPR, the noise energy normalizes more in people who also practice voice therapy, in comparison to the people who only take the medications.
The Conclusion
Laryngopharyngeal reflux (LPR) is a condition in which the digestive acids in your stomach flow back up the throat to the voice box and pharynx. This can cause damage to the throat and vocal cords.
Several factors such as obesity, low stomach acid, problems in LES, or overgrowth of bacteria in the small intestine can cause LPR.
Practicing dietary and lifestyle changes under the guidance of your doctor can help relieve symptoms of LPR.
