
If you are feeling a sudden weakness or light-headedness, Hypoglycemia can be the cause. Commonly referred to as ‘low blood sugar’, this tends to occur in people with diabetes.
You may experience dizziness, intense hunger pangs, or as if the energy has suddenly been sucked out of your body. Some people even faint when their blood sugar drops abruptly.
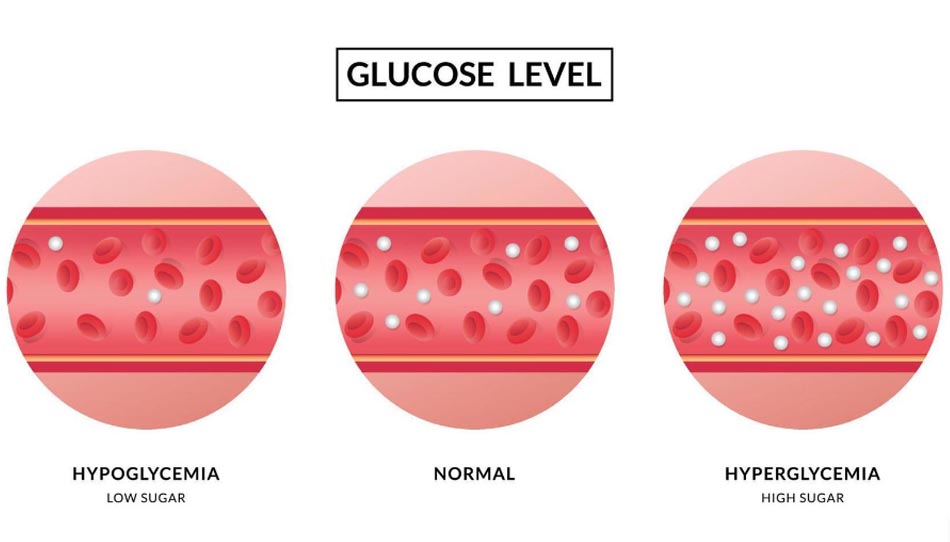
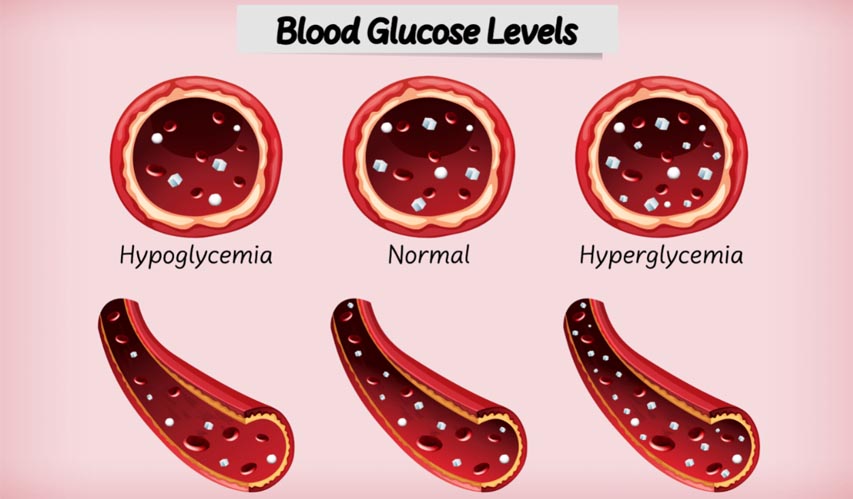
Glucose is the primary energy source that our body uses to fuel all its functions. You get hypoglycemia when your body does not have enough glucose to use as fuel. This can happen due to several reasons, including medication and diet.
It is important to recognize the symptoms of hypoglycemia and take action immediately. Hypoglycemia is preventable if you understand what causes it and follow the necessary precautions.
What is hypoglycemia?
Hypoglycemia is a condition in which your blood sugar level drops below 70mg/dL or 3.9 mmol/L. Hypo means low or under and glycemia means glucose or sugar in your blood (1). Therefore hypoglycemia means low blood sugar.
What causes hypoglycemia?
Hypoglycemia can happen due to many reasons such as:
- An overdose of medications raises insulin levels in the body. This is the most common cause of hypoglycemia.
- Skipping meals, or
- Eating too little leads to low sugar levels in your body.
- Intense exercise can deplete glucose levels in your blood
What can cause hypoglycemia in non-diabetics?
In non-diabetics, the causes of hypoglycemia include:
- Binge-drinking alcohol
- Certain illnesses of the liver
- Pancreatic tumor
What is the relationship between glucose and insulin levels?
Glucose comes from food, especially carb-rich foods. When you eat food, it is broken down into glucose that is absorbed in the bloodstream and is available to the body cells.
Insulin is a hormone secreted by the organ, pancreas. It helps these cells to uptake glucose for energy. It is a very important process that enables the body to function.
Therefore, for some reason, if this glucose drops below normal, the body fails to work properly. This leads to low blood sugar or hypoglycemia and needs immediate treatment or else can lead to other complications.
Our brain is permanently dependent on glucose. Therefore, our body has a strong counter-regulatory response to hypoglycemia that quickly increases the glucose levels in response to the sugar drop. However, if there is an unbalance in this system, the body experiences hypoglycemia that needs attention (2), (3), (4).
Common symptoms of hypoglycemia (low blood sugar)
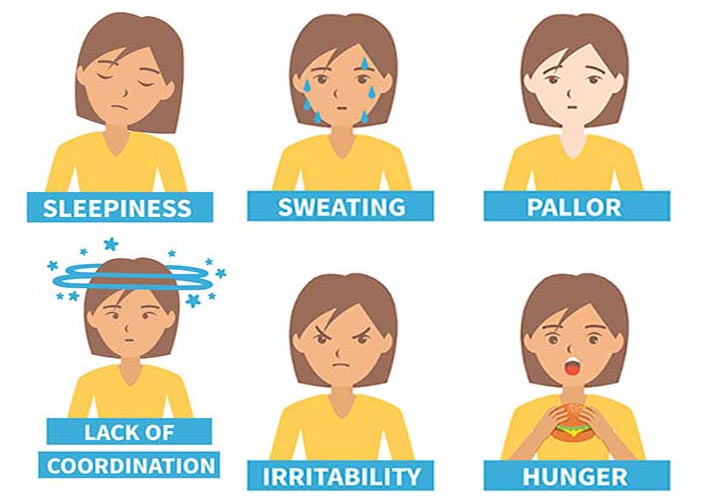
Signs and symptoms of hypoglycemia are (5), (6):
- Weakness
- Shakiness or Tremors
- Dizziness
- Blurry vision
- Nausea
- Vomiting
- Hypoglycemia muscle cramps
- Lightheadedness and chills
- Palpitation or rapid heart rate
- Confusion
- Headache
- Hunger
- Confusion
- Slurred speech
- Irritability or crankiness
- Skin tingling and itching
- Anxiety
- Shortness of breath
Please keep in mind that hypoglycemia can be a medical emergency. If you or someone you know is showing the symptoms and the person is not responding to the initial steps, immediate action must be taken (which we will cover shortly).
What are the different types of hypoglycemia?
There are two main types of hypoglycemia:
- Diabetic hypoglycemia
- Non-diabetic hypoglycemia
- Reactive
- Non-reactive
Hypoglycemia is also categorized into:
- Fasting hypoglycemia
- Age-based hypoglycemia
- Newborns/neonatal
- Infants
- Toddlers
- Elderly
- Time-based hypoglycemia
- Morning
- Afternoon
- Night
Now let’s take a deeper look at each of these categories of hypoglycemia.
1. Diabetic hypoglycemia
Causes: When hypoglycemia occurs in diabetic people as a side effect of the medication that they are taking, it is known as diabetic hypoglycemia (7). It is mainly caused while taking insulin or medications that increase insulin production. The other common causes of hypoglycemia in diabetic patients are:
- Missing meals or missing meal after medication
- Not eating enough
- Alcohol intake
- A sudden increase in exercise without adjusting the medication
Treatment: In case you see the telltale signs of blood sugar drop, eat or drink sugar or carbohydrate-rich food to raise the levels quickly. Glucose tablets and gels are also available that can provide instant energy. Remember to not have sugary products that have fat. It will slow down the rise of blood sugar.
2. Non-diabetic hypoglycemia
Two types of hypoglycemia can occur in people who are non-diabetic. They are:
- Reactive hypoglycemia
- Non-reactive hypoglycemia
Reactive hypoglycemia
This kind of hypoglycemia is also known as postprandial hypoglycemia and can occur within 4 hours after a meal (8).
Diagnosis: Doctors diagnose reactive hypoglycemia in the following ways:
- Asking you about the signs and symptoms.
- Taking a blood sample while having the symptoms to check on the blood glucose level.
- Checking to see whether the symptoms ease after the treatment when the blood glucose level reaches 70mg/dL.
If the blood glucose drops lower than 70mg/dL while experiencing the symptoms and you get relief when the glucose level gets raised after drinking or eating, the diagnosis is confirmed.
Causes of reactive hypoglycemia
The causes of reactive hypoglycemia are still debatable.
- Some studies state that certain people can be more sensitive to the hormone epinephrine, which is normally released by the body. This can cause hypoglycemia (9).
- Other researchers state that a deficiency in glucagon secretion can lead to reactive hypoglycemia (10).
- Gastric bypass surgery or bariatric surgery may also cause reactive hypoglycemia. This happens because of the rapid passage of food in the small intestine which doesn’t allow enough time for the food to digest properly (11).
- Enzyme deficiencies such as hereditary fructose intolerance which are rare and known as enzyme deficiency hypoglycemia can also be the cause (12).
Fasting hypoglycemia
Fasting hypoglycemia, also known as postabsorptive hypoglycemia is mainly due to an underlying disease.
Diagnosis: Fasting hypoglycemia is diagnosed from a blood sample that shows a blood glucose level below 50mg/dL after an overnight fast, between meals, and after physical activity (13). These periods are specially chosen because of the lengthy time duration when the body is in a fasting state or rapid glucose absorption state.
Causes of fasting hypoglycemia
Fasting hypoglycemia may happen because of:
1. Certain medications: Drug-induced low blood sugar is the lowering of the blood sugar levels resulting from medications. Medicines that cause hypoglycemia are beta-blockers, heart arrhythmia medicines such as cibenzoline and quinidine, certain pain relievers, insulin, metformin when used with sulfonylureas, SGLT2 inhibitors, sulfonylureas, and drugs that fight infections such as gatifloxacin. Studies have also stated that the antimalarial drug quinine has been closely associated with life-threatening hypoglycemia (14).
2. Alcoholic beverages: Fasting hypoglycemia can also be caused by alcohol consumption, especially binge drinking. Alcohol metabolism in the body interferes with glucagon metabolism. The later metabolism is especially important as it raises the blood glucose level as per the body’s requirement (15).
3. Critical illness: The organs that are directly responsible for maintaining the blood glucose level in the body are the liver, heart, and kidneys. Any illness affecting these organs can also cause hypoglycemia (16). Other causes are sepsis and eating disorders where your body starves for a prolonged period of time.
4. Hormonal deficiencies: A common reason for fasting hypoglycemia mainly in very young children is a hormonal deficiency. This is especially true for growth hormones, cortisol, glucagon, or epinephrine. Studies have also linked hypothyroidism with certain biochemical and nervous system abnormalities that can cause hypoglycemia (17). This condition is linked to low growth hormone and cortisol responses to insulin-induced hypoglycemia.
Hormonal tests can confirm this kind and often hormone replacement therapy can help solve it.
5. Certain tumors: Insulin-producing tumors in the pancreas called insulinomas can also be one of the biggest reasons for fasting hypoglycemia. As these tumors raise insulin levels, the blood sugar drops very fast causing hypoglycemia. Lab tests can confirm the same and medical or surgical treatment to remove the tumor can correct the problem.
6. Conditions occurring in infancy and childhood: Hypoglycemia in children is normally not very common. However, if it occurs, the reason is mainly hyperinsulinism, enzyme deficiencies that regulate carbohydrate metabolism, and hormonal deficiencies such as a lack of pituitary or adrenal hormones.
Age-based hypoglycemia
Neonatal hypoglycemia or Hypoglycemia in newborn
Neonatal hypoglycemia is a condition when the blood glucose level is less than 30mg/dL in the first 24 hours of the life of the newborn. Hypoglycemia in the newborn is evident from certain signs. Blue lips and skin, pallor, hypothermia, poor muscle tone, apnea, and shakiness are to name a few (18).
If not treated, in the long run, it can lead to neurological damage resulting in mental retardation, recurrent seizure activity, developmental delay, and personality disorders. It may also impair cardiovascular functions and can cause serious brain injury.
The causes of blood sugar dropping in newborns are:
- Poor nutrition of the mother during her pregnancy period
- Poorly controlled diabetes of the mother
- Incompatible blood types of mother and baby
- Birth defects
- Birth asphyxia
- Congenital metabolic diseases
- Tumor of the pancreas
- Preterm babies with incomplete development of organs
- Small or large for their gestational age
- Born under lots of stress
- Growth hormone or cortisol deficiency can stop the production of glucose in the liver which can result in low blood sugar hypoglycemia. In case the hypoglycemia goes beyond the first 48 hours of life, it is termed persistent neonatal hypoglycemia. One of the leading causes of this is hyperinsulinism
Hypoglycemia in infants
Pediatric hypoglycemia can affect anyone from newborns to adolescents. However, it is more common among newborns and infants. Normally blood glucose levels are maintained at 55-60mg/dL after birth. However, this increases to 70mg/dL at approximately 2 days of life. In case, the levels are too low, it is said to be hypoglycemia, and intervention is given (19).
Causes
- Low fat and glucose stores
- Health issues such as fever, seizure, and stress can raise the need for glucose in the body
- Having other health issues such as hemolytic disease
- Birth defects or genetic problems
- Illegal drug use by the mother
- Mother having high blood pressure
As mentioned earlier in the section on neonatal hypoglycemia, infants who are born too large or small, born preterm or post-term, or born to mothers with diabetes are at risk of hypoglycemia.
Hypoglycemia in toddlers and children
Hypoglycemia is common in newborns, however, it is not the same for older children. In case they have, it is most often a complication of insulin therapy for diabetes. For the majority of them, hypoglycemia is temporary and easily treated. However, there are some rare disorders in which hypoglycemia is recurrent and potentially life-threatening.
The most common cause of mild or severe hypoglycemia in children is insulin-treated type-1 diabetes when there is a mismatch between food, exercise, and insulin (20).
Young children who do not have diabetes can also experience hypoglycemia. Single episodes can be seen while:
- Stomach flu or some illness where the food intake reduces a lot while the output is constant
- Fasting for a prolonged period of time
- Prolonged strenuous exercise that causes exercise-induced hypoglycemia
However, if the episodes are recurrent, then the reasons might be (21):
- A congenital error in metabolism or unusual disorder such as hypopituitarism or hyperinsulinism.
- Accelerated starvation, also known as ‘ketotic hypoglycemia.’
- As a side effect of some medication that your child is taking.
Hypoglycemia in elderly

The elderly are prone to having hypoglycemia due to several factors (22), (23), (24). They can be:
- Lifestyle-related – such as dietary error, alcohol intake, and excessive physical activity.
- Drug-related – which includes wrong dosage, wrong time, and technique of administration.
- Medical disease related – to renal, hepatic, and /or gastrointestinal dysfunction.
- Endocrine-related diseases – such as hypothyroidism, hypopituitarism, and hypoadrenalism.
- Nervous systems related – such as cognitive impairment, autonomic neuropathy, and gastrointestinal neuropathy.
Time-based Hypoglycemia
Morning Hypoglycemia
People with diabetes experience too much long-acting insulin also known as background insulin or basal insulin. This may result in low blood sugar in the morning.
People who do not have diabetes can also experience low blood sugar because of their defective diet and exercise habit. Some of the other causes of morning hypoglycemia can be:
- Chronic starvation
- Too much alcohol the previous morning
- Severe liver or pancreas disease
Hypoglycemia in the afternoon
Throughout the day, our body is consuming glucose to provide energy for optimum functioning. However, sometimes there is an afternoon sugar crash. You are suddenly hit by fatigue and can barely keep your eyes open. Even though you feel that it’s the cup of coffee that you need, actually you are undergoing low blood sugar or afternoon hypoglycemia.
If you want to prevent such episodes, the food that you eat in your lunch should have the following:
- A good source of anti-inflammatory, plant-based oil
- Complex carbohydrate and fiber-rich food
- High-nutrient, low-glycemic vegetables
- High-quality protein
Hypoglycemia in the night ( Nocturnal hypoglycemia)
Nocturnal hypoglycemia is a condition in which your blood glucose levels are typically below 63 mg/dL while sleeping at night. It is believed that more than half of the severe episodes of hypoglycemia take place at night. It is estimated that 50% of children with Type-1 diabetes (TIDM), especially kids aged below 7 years. Sudden nocturnal deaths are also known as “death in bed”. This is attributed to nocturnal hypoglycemia (25).
It can be extremely dangerous. People who are more at risk are:
- The ones taking slow-release insulin at night that become effective six to eight hours after each dose
- Increased physical activity before bedtime
- People who skip meals, especially dinner, or longer time intervals between meals
- Have some kind of infection
- Counter regulatory mechanisms
Warning signs
- Restless sleep
- Clammy and sweaty skin
- Shaking
- Change in breathing
How is hypoglycemia in general diagnosed?

A blood glucose meter is usually used to test your blood sugar levels. If the reading shows below 70mg/dL, start treatment accordingly. This mainly means lowering the potency of the drug that you are taking as a diabetic.
However, if you are not on any medication, then your doctor will ask you the following questions to determine the cause:
- The blood sugar level while you were experiencing hypoglycemia
- Does the symptom disappear when the blood sugar level increases
- What are the exact signs and symptoms?
What is the treatment for hypoglycemia?

The most common practice for hypoglycemia is the 15-15 rule. This means you should have 15 grams of carbohydrates to raise your blood sugar and check it after 15 minutes. If it’s below 70mg/dL, go for another serving.
Keep repeating till your blood sugar is at 70mg/dL. Once your sugar levels are back to normal eat your meal so that you can maintain that range.
The foods that can help raise blood sugar levels after a bout of hypoglycemia episode are:
- Four glucose tablets
- A serving of glucose gel
- Five to six pieces of hard candy
- Four ounces of fruit juice
- One tablespoon of either sugar, honey, or corn syrup

After your blood sugar level comes back to normal, have a nutritious snack or meal to avoid the level dropping again.
Emergency treatment
If the above treatment doesn’t work, you should be using a glucagon kit. Glucagon is a hormone whose function is exactly the opposite of insulin. It helps raise blood sugar quickly. It can be a lifesaver for a person who isn’t alert enough to eat or drink something.
Keep in mind that glucagon is available only by prescription. The kit comes as an emergency syringe kit or as a nasal treatment. When given to someone who is unconscious, the person should be turned on his or her side to prevent choking in case of vomiting. If this doesn’t work either, call emergency medical care asap.
Treatment for the underlying cause
If the hypoglycemia is happening often i.e., recurring quite frequently, it is known as recurrent hypoglycemia. This can be identified by your doctor by assessing your condition, signs, and symptoms. Depending on the cause, your treatment will be:
- Medications: If your hypoglycemia is because of the medicines you are taking, your doctor may want to adjust the dosage and check on you. If the hypoglycemia persists, he will change or stop it altogether.
- Tumor treatment: If the cause of your hypoglycemia is a tumor in your pancreas, then a partial or complete surgical removal is necessary.
How can you prevent hypoglycemia?
- Monitor your blood sugar regularly
- Do not skip meals
- Eat small meals and snacks every 3 hours
- Make sure you take the proper dosage of your medication and not more. Measure medications carefully before taking them.
- Be physically active and plan your food accordingly so that you do not experience episodes of sugar drop
- Eating foods high in fiber, protein, good fats, and complex carbohydrates can keep digestion proper and the body’s ability to maintain the sugar balance
- Limit high sugar, refined, and processed food, especially on an empty stomach
A registered dietitian can give you your own personalized diet chart and proper meal-planning advice. Most health professionals recommend a high protein and low carbohydrate diet to treat hypoglycemia.
Severe hypoglycemia
Hypoglycemia can be mild, moderate, or severe. This is mainly based on the person’s blood glucose and condition (26).
- Level 1 (mild) hypoglycemia: Blood glucose level less than 70 mg/dL but above 54 mg/dL.
- Level 2 (moderate) hypoglycemia: Blood glucose level goes below 54 mg/dL
- Level 3 (severe) hypoglycemia: Blood glucose level goes below 40 mg/dL. During this phase, a person is unable to function and needs another person’s help.
Severe hypoglycemia mostly occurs in people with diabetes who take insulin or certain diabetes medication mainly sulfonylureas. It is mostly seen in people who have type-1 diabetes since they need to take multiple insulin injections daily. It may occur in type-2 diabetics also who take insulin. Severe hypoglycemia is preventable when in consultation with your doctor and taking the required steps.
Severe hypoglycemia can be life-threatening and is considered an emergency.
Hypoglycemia unawareness

Hypoglycemia unawareness, also known as impaired hypoglycemia unawareness, is a condition that occurs due to complications of diabetes. The patient is unaware of the blood sugar drop as it fails to trigger the secretion of epinephrine which is responsible for the characteristic symptoms of hypoglycemia (27).
As the patient does not experience or perceive the symptoms, he does not get the warning signals from the body. If remains untreated, hypoglycemia unawareness results in severe hypoglycemia complications. Because of the prolonged exposure of the body to hypoglycemia, can result in seizures, loss of consciousness, brain damage, or even more.
High-risk category people for hypoglycemia unawareness
About 1 in 5 people with type-1 diabetes and 1 in 10 people with type-2 diabetes who take insulin experience hypoglycemia unawareness.
Going low while sleeping: Some people experience hypoglycemia at night and as they are asleep, can’t perceive the symptoms. If it continues in a frequent manner, it can affect the body’s ability to detect hypoglycemia warning symptoms while awake.
Exercise: Chances of hypoglycemia increase during and after exercise as the body’s tissues are more sensitive to insulin. This can occur up to 15 hours later, especially after strenuous exercise.
Having diabetes for a long time: Studies have observed that 50% of people who have used insulin for more than 20 years develop impaired hypoglycemia unawareness.
Age: With the decline of cognitive functions as you age, the recognition of the hypoglycemic symptoms reduces. Some studies have shown that hypoglycemia unawareness occurs more frequently in people above the age of 60.
Alcohol Consumption: Alcohol intake can also lower your understanding of hypoglycemic symptoms. It can also impair the liver’s functioning resulting in the inability of the liver to release glucose when the blood sugar is too low.
Certain prescription drugs: Non–selective beta-blockers that are used to manage high blood pressure can reduce your ability to recognize hypoglycemia. Some medicines used to treat depression can also reduce your ability to treat hypoglycemia.
Frequently Asked Questions (FAQs) on Hypoglycemia
1. How long do people have hypoglycemia?
It usually depends upon the factor that caused it. Hypoglycemia due to taking long-acting insulin or sulfonylurea takes one to two days to go away. However, people with diabetes remain at risk always as they take medications to lower blood sugar.
Simple changes in your lifestyle such as diet and eating schedule can resolve episodes of hypoglycemia. This way they can be prevented. A balanced and stable diet that is low carb, and high in protein and fiber can definitely help you.
2. How can you have hypoglycemia after meals?
Hypoglycemia after a meal is also known as Reactive hypoglycemia. It usually takes place within 4 hours after eating. The main cause is the body’s high production of insulin. This usually happens after a large, carb-heavy meal. For reasons unknown, the body continues to secrete extra insulin even when the food is digested resulting in a blood glucose drop.
3. What causes hypoglycemia in pregnancy?
The factors that can cause hypoglycemia in pregnancy are:
- You are not eating enough. This is because the baby is continuing to siphon glucose from your body and it needs to be compensated continuously with healthy food.
- Excessive exercise is depleting your blood sugar levels and you are not fast enough to replenish it
- Your diabetes medication doses are more potent or the dosage is higher than what your body needs
4. What is insulin-induced hypoglycemia?
Insulin-induced hypoglycemia is low blood glucose levels due to the intake of insulin or insulin-producing medication. This mainly happens in diabetics (28).
5. What is persistent hyperinsulinemic hypoglycemia of infancy (PHHI)?
Persistent Hyperinsulinemic Hypoglycemia of Infancy (PHHI) is one of the most common causes of severe, persistent, neonatal hypoglycemia. It is a rare genetic disorder that results due to inappropriate and unregulated insulin secretion in the face of severe hypoglycemia (29).
6. What is idiopathic hypoglycemia?
Idiopathic reactive hypoglycemia (IRH) describes a condition where recurrent episodes of symptomatic hypoglycemia occur one to four hours after a meal, usually a very high-carb diet. It is synonymous with reactive hypoglycemia or hypoglycemia which is not diagnosed by a physician and doesn’t fulfill the Whipple triad criterion (30).
This condition is also known as idiopathic postprandial syndrome.
7. What is ketotic hypoglycemia?
Ketotic hypoglycemia occurs in children between the age of 10 months and 6 years. It is a condition in which the lowering of blood glucose is accompanied by ketosis and often vomiting in young children. Ketotic hypoglycemia nearly always occurs in the morning after an overnight fast especially if it is longer than usual. The blood glucose level is usually found to be between 35-60mg/dL. Precipitating factors can also be a low carbohydrate intake the previous day or stress such as viral infection (31).
8. What is non-ketotic hypoglycemia?
Non-ketotic hypoglycemia may be caused due to fructose or galactose metabolic disorder in the body. It can also be associated with hyperinsulinism, fatty acid oxidation, and GH deficiency (32).
9. What is neuroglycopenia?
The shortage of glucose in the brain due to hypoglycemia is termed neuroglycopenia. It is actually glucopenia of the neurons. This condition affects the function of the brain cells. Symptoms are usually warmth, weakness, difficulty, confusion, and drowsiness. Prolonged or recurrent neuroglycopenia can result in loss of consciousness, brain damage, coma, and sometimes death (33).
10. What is auto-immune hypoglycemia?
Insulin autoimmune syndrome (IAS) is an uncommon cause of hyperinsulinemic hypoglycemia or auto-immune hypoglycemia. It happens when the body makes antibodies to attack insulin. As insulin is crucial in keeping your blood sugar at a normal level, so when it is attacked the insulin starts working overtime resulting in too much insulin causing hypoglycemia (34).
IAS is the third leading cause of spontaneous hypoglycemia. Recently it has been increasing steadily in the non-Asian population as well leading to recurrent hypoglycemia.
11. What is Whipple’s triad criterion for hypoglycemia?
Whipple’s triad is a collection of three criteria that examines a patient’s symptoms resulting from hypoglycemia that may indicate insulinoma, a pancreatic tumor.
Final Note

Hypoglycemia is a sudden drop in your blood sugar level. It can lead to dizziness, extreme weakness, and in some cases fainting. It is more common among diabetic patients who are taking insulin or insulin-producing medications.
However, hypoglycemia can also occur in non-diabetic people. The cause of low sugar in the body can be anything from binge drinking to a pancreatic tumor.
Hypoglycemia is seen not just in adults, but also among newborns and infants. Therefore, it is important to recognize the symptoms and take treatment accordingly.
