
Most of us have experienced acid reflux at some time or the other, especially after a heavy or spicy meal.
This happens when the stomach acid flows back to the esophagus, a tube from your throat to your stomach. The resulting burning sensation in the lower chest area is commonly known as heartburn.
Acid reflux is totally normal once in a while. In fact, one in five people experiences heartburn or reflux on a weekly basis. Two in five people have heartburn or acid reflux at least once a month. But, if its occurrence becomes frequent, you may have developed GERD (Gastroesophageal Reflux Disease).
Proper lifestyle changes and timely interventions can help improve gastroesophageal reflux and send it into remission. Keep reading and understand the root cause and effective treatments for acid reflux.
What is acid reflux?
Acid reflux, also known as gastroesophageal reflux (GER) is the backwash or regurgitation of stomach acid into your food pipe (esophagus). This causes irritation to the lining of the esophagus, manifesting itself as pain in the center of the chest behind the sternum. This sensation of heartburn is one of the most common symptoms of acid reflux (1), (2), (3), (4).
Heartburn is sometimes called acid indigestion or pyrosis. Often, it is an acute problem when there is sudden gastric reflux. This acute acid reflux can be managed well with proper intervention.
Acid reflux and gastroesophageal reflux disease or disorder (GERD) are not the same. When you experience mild acid reflux at least twice a week or severe acid reflux at least once a week, it is Gastroesophageal reflux disease (GERD). GER is a normal physiologic process while GERD brings with it troublesome symptoms.
In some countries, the esophagus is spelled as the esophagus, and GERD is referred to as GORD.
In GERD, the stomach acid persistently flows back up into your mouth. Also known as chronic acid reflux, GERD is an advanced form of acid reflux (5).
Acid reflux comes in four stages which include stage 1 with mild symptoms, stage-2 with moderate symptoms, stage-3 with severe GERD symptoms, and stage-4 which results in reflux-induced precancerous lesions or esophageal cancer.
Symptoms of acid reflux and GERD
GERD is one of the common gastrointestinal disorders that affect the stomach, esophagus, and often the throat.
Acid reflux and GERD typically show symptoms of:
- Heartburn and
- Regurgitation
It can also present atypical symptoms which are manifested as ear, nose, throat, cardiac and pulmonary symptoms (6), (7), (8), (9), (10). The acid in the throat and chest results in:
- Lump in the chest
- Heartburn on the upper chest
- Heavy chest
- Dental erosions
- Laryngitis asthma
- Chronic dry cough
- Dysphagia (the sensation of food being stuck in the throat)
- Sore throat
- Difficulty swallowing
The other symptoms are:
- A sour or bitter taste at the back of your mouth
- Bloating
- Swollen stomach
- Dry throat
- Wheezing sound and chronic sore throat
- Burping
- Coughing up phlegm
- Sinus and headache
- Belching
- Stomach cramps
- Chest discomfort
- Nausea
- Hiccups
- Chest pain and shortness of breath
What causes acid reflux?
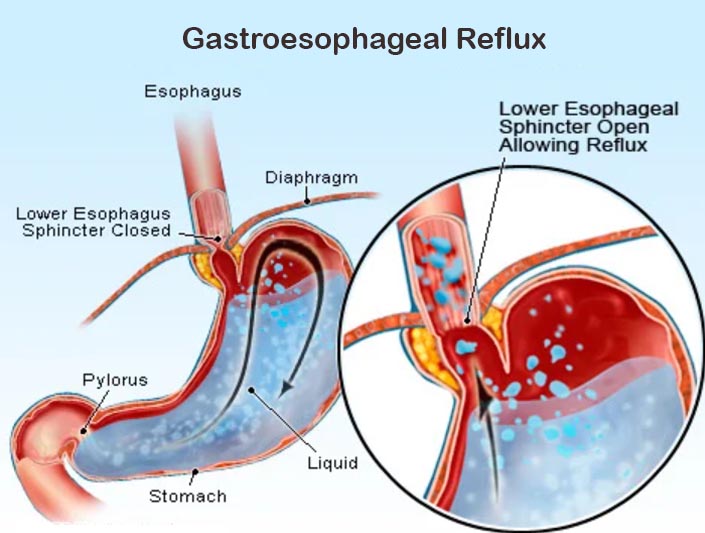
Your stomach is a muscular, J-shaped organ that helps in the digestion of food. At the entrance of your stomach is a ring of muscle called the lower esophageal sphincter (LES), which acts as a valve. It is a 3-4 cm tonically contracted smooth muscle segment that separates the esophagus from your stomach.
Normally, LES closes as soon as food passes through it. LES acts as a drawstring that closes off the opening when the stomach is full. This prevents the stomach acid from moving up. In people with acid reflux or GERD, the LES doesn’t close completely.
Even though the lining of the stomach can handle the acid, the same is not true for the esophagus or larynx. Therefore, the regurgitation can cause heartburn and chest discomfort (11). Factors that loosen the LES are:
- Foods and drinks such as fatty foods, alcohol, caffeine, and excess chocolates.
- Smoking
- Body’s position while sleeping
- Something that increases the pressure in the stomach and forces the stomach acid backward such as pregnancy
- Medical conditions
- Side effects of certain prescription medicine
The factors that cause acid reflux and GERD
Acid reflux and GERD causes can be (12):
Hiatal Hernia
The diaphragm is a muscle that separates the stomach from the chest. It lies in the abdomen and is mainly used to help breathe. In a hiatal hernia, the upper part of the stomach pushes up through your diaphragm. The hole or opening through which it moves up is called hiatus, hence the name.
Usually, the diaphragm helps keep acid in our stomach, but in a hiatal hernia, acid can move up into your esophagus and cause symptoms of acid reflux disease.
Malfunctioning of LES
If a person’s LES is weak or damaged, the muscle can lose its ability to open or close properly. When that happens, the stomach acid splashes up from the stomach into the esophagus, causing severe acid reflux.
Pregnancy
Acid reflux is very common in pregnancy. It is caused because of the hormonal changes that the pregnant lady goes through. More so in the later stages of pregnancy, when the growing uterus and fetus put increased pressure on the stomach. This pressure causes acid to leak, especially after a meal when the stomach is full causing acid reflux.
Obesity
Obesity leads to an increase in intra-abdominal pressure that can cause acid reflux. According to the American Society For Gastrointestinal Endoscopy, obesity is one of the leading causes of acid reflux. Visceral obesity increases the pressure over the gastroesophageal junction leading to reflux.
Smoking (both active and passive)
Smoking and acid reflux go hand in hand. Smokers have experienced waking up in the middle of the night with acid in their throats. Some have permanent damage to their throat leading to hoarseness. Smoking contributes to GERD by:
- Relaxing the LES: The nicotine from tobacco present in cigars and cigarettes can relax the LES, allowing the stomach acid and digestive juices to go back into the esophagus causing severe heartburn and other complications.
- Increasing stomach acidity: Smoking and stomach acid are directly linked. Smoking prompts the stomach to produce more acid causing hyperacidity. This excess acid causes smoking heartburn.
- Reducing salivation: Saliva contains bicarbonate, a substance that can neutralize acid and help fight the effects of acid reflux and GERD.
- Damages the esophageal lining: The mucus membrane offering a protective coat on the esophagus is damaged by smoking resulting in worsened symptoms.
- Interferes with esophageal muscles: The stomach muscles that help move the food from the esophagus to the stomach are damaged from smoking. As a result, the chances of reflux increase manifold.
Stress and anxiety

Studies have observed that stress can deplete the production of prostaglandins, substances that normally protect the stomach from the effects of acid.
This can be one of the factors that increase your perception of pain and discomfort. That is stress and anxiety, cause changes in the brain that turn up pain receptors making you more sensitive. Stress can also decrease the production of stomach acid which is a leading cause of acid reflux (13).
It aggravates more when you are tired. Stress coupled with exhaustion can lead to changes that increase acid reflux.
Alcohol
Alcohol can increase the symptoms of GERD or acid reflux and causes damage to the esophageal mucosa (14). Therefore, GERD patients are recommended to avoid alcohol or to switch to moderate consumption.
Nutrient deficiencies
- Zinc deficiency: Zinc deficiency caused by inadequate dietary intake or by nutrient loss can cause low stomach acid that leads to acid reflux.
- Potassium deficiency: Potassium helps in muscle movement and the nerves to send their signals. Since LES is a muscle, potassium deficiency can lead to its loosening, resulting in incomplete closure.
- Vitamin B deficiency: Especially vitamin B3 and vitamin B12 deficiency can cause low stomach acid.
- Vitamin D deficiency: Vitamin D controls muscle functions. When we are dealing with the stomach, we are looking into smooth muscles. The sphincters and the muscles. As vitamin D helps in the absorption of calcium, its deficiency can result in less calcium. This mineral helps in contractility. Vitamin D and calcium deficiency, therefore, leads to incomplete closure of the valve resulting in regurgitation.
- Others: Chloride, sodium, and iodine deficiency are crucial in producing adequate levels of stomach acid (HCl). Therefore, a deficiency of these minerals can be an important factor leading to acid reflux. If the acid content is low, the pH is not acidic enough. This results in incomplete closure of LES leading to acid reflux.
Achlorhydria or hypochlorhydria
The main purpose of the stomach is to break down protein and absorb minerals such as calcium, iron, and potassium. The pH of the acid is low and it’s an acidic environment out there. This acidic stomach is important to optimize the work of the digestive enzymes and to kill off bacteria and viruses.
But when stomach acid is low, as in the condition called hypochlorhydria, the food is not broken down properly. The more time this food lay there in the stomach, the more they are exposed to bacterial infestation. This causes increased gas production mainly hydrogen and methane that leads to bloating and belching eventually resulting in acid reflux.
Low stomach acid can lead to low pancreatic enzymes that result in incomplete digestion and increase the chances of acid reflux even more.
Bariatric surgery
Gastric bypass and sleeve gastrectomy, are the two most common bariatric surgeries. This is performed especially to alleviate GERD. However, sometimes it is possible to have GERD after surgery. In that case, talk to your doctor who can help you find the correct treatment.
Low bile
Bile is a substance that is produced by the liver and stored in the gallbladder to be secreted when needed. Bile is mainly used to break fats. It helps you break down fat and extract fat-soluble vitamins. It also helps absorb healthy fats.
Low bile enzymes will cause improper digestion resulting in acid reflux. It can happen because of liver problems.
Hypothyroidism
Hypothyroidism can lead to acid reflux, due to many factors.
- The thyroid hormone plays a crucial role in hydrochloric acid secretion. Therefore, hypothyroidism can be a big cause of low stomach acid (hypochlorhydria) or no hydrochloric acid (achlorhydria) that causes acid reflux (15).
- Poor digestion and absorption of essential nutrients such as calcium and vitamin D lead to poor stomach acid.
- Hypothyroidism also decreases gastroesophageal motility (16).
Infections and diseases
Some infections such as Helicobacter pylori infection, diseases such as pernicious anemia, and stomach cancer can be the cause of low stomach acid resulting in acid reflux.
Any infection or disease of the pancreas also can be the cause. Bacterial growth in the small intestine (SIBO) is one more on the list of causes of GERD. The gas produced by the bacteria residing in the small intestine can push the stomach acid from the stomach into the esophagus (17).
Certain medications
Medicines such as aspirin, Tylenol, ibuprofen, certain muscle relaxers, and some antihypertensive drugs can lead to acid reflux disease. A few sedatives and asthma medications can also cause acid reflux.
Antidepressants such as Xanax are one more. Antibiotics can irritate the lining of the stomach and can cause hyperacidity in the stomach. Birth control pills or oral contraceptives have also been shown to develop acid reflux (18).
Age-based acid reflux or GERD
GERD can occur in all age groups from babies to teenagers. In fact, one-fourth of all children and teenagers experience symptoms of GERD.
Acid reflux in newborns and infants

Infants very commonly develop acid reflux. As their stomachs are small, being full can easily make them regurgitate. Around 70 to 85 percent of newborns experience regurgitation during the first two months of life. The condition peaks when they are 4 months old.
Also known as newborn acid reflux, 95 percent will outgrow the symptoms about the time they are 12-18 months old. When a baby spits up or vomits, it is not GERD. They are likely displaying gastroesophageal reflux (GER) which is common and is not accompanied by any other symptoms. It is rare for an infant’s symptoms to continue past 24 months. If the condition persists, then it’s a sign of GERD in babies.
Children with developmental and neurological conditions like cerebral palsy can have acid reflux or GERD for a prolonged duration. Symptoms of GERD in children are bad breath, irritability during feeding, hiccups, failure to gain weight, disturbed sleep, chest discomfort, abdominal discomfort, and frequent respiratory infections. GERD in babies is more common in the age group of 2-3 years.
Acid reflux in toddlers and children
5-10% of children in the age group of 3-17 years experience some or the other symptoms of GERD. Children with GERD report different symptoms than adults. It can be anything from a general tummy upset to vomiting or an ear-nose-throat disorder. As children grow old, the prevalence of GERD symptoms increases. With age, the symptoms become more like those found in adults.
The treatment options available for GERD in children are diet modification, smaller meals, and maybe medication to give relief from the symptoms. It is very rare to consider surgery as a treatment for pediatric GERD though.
According to Johns Hopkins Children’s Centre, the complications of pediatric GERD can be respiratory problems, difficulty gaining weight or consistent weight loss, and esophagitis (inflammation of the esophagus). GERD in toddlers and children are more serious than stomach ache or spitting up.
Acid reflux in the elderly
The physiological changes experienced by the elderly make them more prone to suffer from GERD. People over the age of 65 are often given medications that can alter the GI tract and can lead to senior GERD.
GERD in the elderly sometimes does not show any symptoms. Their pain receptors might not be as sensitive due to decades of acid reflux barring occasional heartburn.
It also complicates the matter as some elderly do not secrete much stomach acid. Therefore, the symptoms can’t be alleviated with antacids. Tests are done for proper diagnosis and correct medical intervention is given.
Acid reflux at different times of the day
Acid reflux can occur at any time of day and even when you are sleeping.
Acid reflux in the morning
Acid reflux or heartburn in the morning was first termed as “riser’s reflux” by a 2009 study where 39 patients with GERD were studied. 19 participants reported acid reflux within the first 20 minutes of waking up in the morning. This was around 50% of the participants. It was concluded that in GERD patients, acid reflux in the morning is quite common.
Sleeping with your body raised from the waist up, 3 hours gap between the last meal and sleep, and avoidance of foods that trigger acid reflux in dinner can be the right solution.
Acid reflux after exercise

Exercise has been known to trigger heartburn if the LES muscle is weak or too relaxed. As you burp, the stomach acid flows back up causing acid reflux. This exercise-induced heartburn can be prevented by following some tips;
- Avoid eating too fast and chew properly the last meal before your exercise
- Avoid trigger foods that loosen or relax the LES
- Eat something soothing before exercise. This should be taken two to three hours before working out
- If certain intense exercise is triggering heartburn, then change it Headstands and downward dog in yoga which reverses the natural gravity of digestion shouldn’t be done especially in a full stomach
Acid reflux while fasting
Acid reflux or heartburn after eating is very common. A big, spicy, fatty meal can trigger it. Acid reflux after eating usually begins 30-60 minutes after a meal. However, fasting can also be the cause of acid reflux.
An empty stomach leads to a reduction in stomach acid which helps food to digest properly. However, the thought or smell of food can trigger the brain into telling the stomach to produce more acid in anticipation. This can lead to heartburn and reflux.
Acid reflux in the night
Acid reflux has been known to be the worst at night for particularly these reasons.
- As you are lying, gravity does not take the acid back into the stomach
- We stop swallowing while sleeping. Normally when you swallow, the saliva helps carry the acid that has refluxed into the esophagus back into the stomach.
Avoid eating too much at night, keeping a gap of 2-3 hours between your meal and sleep can help manage acid reflux at night.
Acid reflux while sleeping
The National Sleep Foundation states that GERD is one of the leading causes of disturbed sleep among adults between the ages of 45 and 64.
The symptoms of GERD while sleeping are mainly coughing or choking. This sensation can also cause you to wake up from sleep. To prevent acid reflux while sleeping it is best to avoid common acid reflux triggers that we will discuss in detail later.
If a prescription medicine such as anticholinergics, calcium channel blockers, tricyclic antidepressants, and nonsteroidal anti-inflammatory drugs (NSAIDs) is the cause of your reflux, consult with your doctor for an alternative treatment.
Risks and potential complications of acid reflux
If acid reflux is left untreated, it can lead to severe GERD attacks and serious complications that include:
- Esophagitis
- Tooth enamel erosion and gum disease
- Asthma
- Esophageal Strictures
- Barrett’s esophagus
- Esophageal cancer
How is acid reflux diagnosed?
Barium swallow (esophagus)
It is a special type of X-ray test that is done to take a close look at the back of your tongue, larynx, pharynx, and stomach. You are made to swallow barium, a chalky white substance, mixed with water. The solution coats the inside of your upper GI tract. As the barium looks white on X-ray film, it helps highlight the area and help the doc diagnose.
Laryngoscopy
Laryngeal findings associated with acid reflux, GERD, or LPR can be assessed with flexible laryngoscopy.
Esophageal manometry
This is a test done to measure the function of the lower esophageal sphincter and the muscles of the esophagus. This test successfully detects if your esophagus is able to move food to your stomach normally. It can successfully identify problems with movement and pressure in the esophagus that can lead to heartburn.
Impedance monitoring
This usually measures the rate of fluid movement along the esophagus and helps investigate and diagnose GERD.
pH monitoring
Gastric pH monitoring can measure the frequency and duration of stomach acid in the esophagus and later how well it clears up from the esophagus. It is normally performed with a thin, plastic tube armed with a sensor that measures the amount of acid backing up into the esophagus.
Intolerance breath test
Hydrogen and methane breath tests are used to explore the pathophysiology of gastrointestinal disorders. SIBO is a condition in which there is bacterial overgrowth in the small intestine. The smell is caused by the fermentation of carbohydrates in the small intestine by bacteria. As SIBO can be a cause of acid reflux or GERD, a proper diagnosis and treatment can relieve the symptoms.
Upper gastrointestinal endoscopy
A thin, flexible tube with a light and camera (endoscope) is inserted down the throat. This examines the inside of your esophagus, stomach, and duodenum, which can detect inflammation of the esophagus or other complications caused by reflux or GERD.
Biopsy
With the above-mentioned procedures, if the doctor wants, they ask for a biopsy test by passing an instrument through the endoscope to take small pieces of tissue from the lining of the esophagus. A pathologist examines the tissue under a microscope and checks for complications. It is also done to detect cancer cells.
Can acid reflux disease be treated with diet and lifestyle changes?

Acid reflux treatments with diet
- Follow a low-carb diet
- Do not eat food that triggers the reflux
- Limit your alcohol intake
- Stop drinking coffee or too many caffeine-containing beverages
- Chewing gums that cause bicarbonate which is known to be effective for GERD
- Do not take carbonated beverages that weaken the LES
- Lessen your chocolate intake as they too weaken the LES
- Avoid mint which has been known to worsen acid reflux symptoms
Foods to avoid for preventing acid reflux are (19):
- Raw garlic, onions, and peppers
- Spices such as chili
- Citrus such as orange, grapefruit, lemon
- Vegetables like cucumber, capsicum, potato, carrots, and tomatoes
- Avocado
- Nuts
- Eggs
- Pickles
- Dairy products like cheese, curd, high-fat content milk
- Corn and lentils
- High-fat foods
- Salt
Foods that are good for acid reflux:
These food have less risk of triggering acid reflux and many of them help reduce acid reflux symptoms.

- Fruits: Bananas, melons, pineapples, apples, and pears are less likely to trigger stomach acid reflux. Bananas are especially very good for GERD. It coats the irritated esophageal lining and helps stop the discomfort.
- Oats: Oatmeal is an excellent source of fiber that is linked to a low risk of acid reflux. Whole-grain wheat and rice can also give you the same effect.
- Lean meats, eggs, and seafood: Chicken, turkey, fish, and seafood can help reduce the symptoms of acid reflux. Avoid egg yolk but egg whites are a good option.
- Whole grains: High fiber in whole grains helps stop symptoms of acid reflux. The high fiber helps absorb stomach acid.
- Sunflower seeds
- Berries especially raspberry and cranberry
- Fermented milk products such as yogurts, Yakult, kefir, and kombucha
Medication for acid reflux relief
1. Antacids: Antacids are drugs that neutralize the acid of the stomach and relieve heartburn. Antacids such as Mylanta, Eno, Gaviscon, Rolaids, and Tums are used to provide instant acidity relief. Even though antacids can provide temporary relief, it is not the solution. In fact, antacids can increase the problem in the long run. Overuse of some antacids also causes side effects such as diarrhea and kidney problems (20).

2. H2 Receptor Blocker: H2 receptor blockers are a class of medicine that are commonly prescribed to treat gastritis, inflamed stomach, and peptic ulcers. All these are the cause of acid reflux. Common H2 receptor blockers are nizatidine (Axid), famotidine (Pepcid, Pepcid AC), and cimetidine (Tagamet, Tagamet HB). These medications are also used to relieve the symptoms of GERD. As the name suggests, these medicines block the H2 receptors in the stomach from producing acids The National Institutes of Health states that these medicines can decrease stomach acid secretion by 70 percent over a 24-hour period. H2 receptor blockers allow time for damaged esophageal tissue to heal as well.
3. PPI (Proton pump inhibitors): PPI medications prevent reflux by blocking the stomach from producing stomach acid. Even though these medications are good for temporary relief, long-term use can be bad leading to serious diseases such as gastric cancer, damage to the liver and kidneys, and nutritional deficiencies (21). One of the most common nutritional deficiencies associated with PPI drugs is Vitamin B12 deficiency.
4. Medications to strengthen LES: Metoclopramide (Reglan) is a prokinetic agent that boosts the motility of the esophagus and stomach and increases the LES pressure. This helps reduce gastric reflux. Prokinetic agents also accelerate gastric emptying.
5. Muscle relaxer: Baclofen is a medicine that can ease the symptoms of GERD by decreasing the frequency of relaxation of the LES. It may cause side effects such as fatigue and nausea (22).
Alternative medicines for acid reflux
Even though studies have not proven alternative medicines to treat GERD or reverse the damage of the esophagus, alternative therapies, and medicines have been shown to bring relief from the symptoms.
Herbal remedies for acid reflux
- Ginger root
- Herbs for GERD such as caraway, German chamomile flower, lemon balm, and milk thistle
- Aloe vera juices
- Fenugreek
- Marshmallow roots
- Licorice roots
- Turmeric
- Saccharomyces boulevard, a probiotic strain specifically for the small intestine, helps optimize the absorption of key nutrients and maximize digestion.
These are best taken naturally. However, supplement forms are also available in the form of teas, oils, and capsules that are believed to give the same benefits.
Relaxation therapies for acid reflux
- Melatonin supplements: Melatonin, also known as the sleep hormone is primarily known to trigger chemical changes in the brain that promote sleep. Studies have confirmed its association with long-term GERD relief.
- Massage: Some studies have observed that massaging the connective tissue around the diaphragm can be a great way of reducing acid reflux for people with GERD. A proper massage can help release the trapped wind that leads to a bloated stomach, flatulence, and acid reflux.
- Acupressure: This procedure has also been shown to bring relief. The key acupressure point in dealing with acid reflux is Pericardium-6 or P6. it is located directly above the wrist. It is believed to stimulate the meridian that directly goes to digestion.
Home remedies for acid reflux

- A glass of lemon juice on an empty stomach in the morning before introducing any food
- One to two teaspoons of apple cider vinegar in warm water
- A tablespoon of baking soda diluted in half a cup of warm water
- Betaine hydrochloride supplements
- Slippery elms help in soothing symptoms of acid reflux such as the sore throat. It also calms the irritation in the digestive tract caused by regurgitation of the stomach content. It comes in the form of a lozenge, capsule, or powder.
- Food allergies and constipation can cause acid reflux. Therefore, pointing out the problem and treating it can relieve you of the cause.
Lifestyle interventions for acid reflux
Lifestyle interventions in acid reflux and GERD can reduce the occurrence as well as symptoms.
- Weight loss
- Moderate physical exercise is good
- High dietary fiber intake
- Avoiding food that causes stomach irritation
- Tobacco smoking cessation
- Do not sleep on your right side which worsens reflux symptoms
- Avoiding late evening meals
- Do not lie down right after your meal
- Chew properly and eat food slowly
- Elevating the head of the bed and sleep
- Avoid tight-fitting clothes
Surgery
Normally acid reflux and GERD can be controlled with medication and by bringing changes in your lifestyle. However, doctors do not recommend their long-term use and may suggest some procedures to get relief. They are:
- Fundoplication
- LINX device
- Transoral incisionless fundoplication (TIF)
- Endoscopy GERD treatment (Stretta)
Frequently Asked Questions (FAQs) on acid reflux
1. What is the difference between acid reflux, heartburn, and GERD?
Acid reflux is a condition in which stomach acid comes up in the esophagus and sometimes the throat and mouth. It ranges from mild to serious. Heartburn is the pain in your chest that occurs as a result of acid reflux. It involves mild to severe pain in the chest and is often mistaken as heart attack pain. GERD is the more severe and chronic form of acid reflux.
2. Can drinking a lot of water cause acid reflux?
Water is neutral with a pH of 7. It is neither acidic nor alkaline. However, water intake in a frequent manner can improve the digestion process and definitely help curb acid reflux or GERD symptoms.
But too much water can disrupt the mineral balance in the body which in turn can lead to acid reflux.
3. Can acid reflux be sent to permanent remission?
Most cases of acid reflux can be cured and go into remission. But keep in mind that this is only true as long as you do not expose your body to the risk factors that caused it. This is especially true for foods that trigger a reaction.
For those with pathophysiological conditions, intervention with medicine can definitely do the needful.
5. How exercise can relieve your acid reflux?
Obesity is one of the biggest factors of acid reflux. Therefore exercise may help prevent or even relieve the symptoms of acid reflux by helping you lose weight.
It also supports proper digestion which combats the root cause of indigestion. However, some exercises in an inverted position may aggravate the already present problem. Therefore the best option is to do low-impact exercises that keep you upright.
6. Is homeopathic medicine effective for acid reflux?
Homeopathic medicines have also been known to relieve acid reflux symptoms. Lycopodium, Natrum carbonicum, Nux vomica, and Pulsatilla are to name a few. They help relieve gastric discomfort, cramps, indigestion, and nausea.
7. Can acid reflux cause asthma?
Asthma and acid reflux often occur simultaneously. Studies have shown acid reflux to worsen asthma. This is mainly because the reflux enters the airways leading to cough, wheezing, and shortness of breath. The same is also true that asthma can worsen acid reflux, especially GERD (23).
The conclusion
Low levels of stomach acid, improper closure of LES, weak sphincter muscles, intense exercise, unhealthy lifestyle, or bad choice of food. Any one of them can be the cause of acid reflux or GERD.
Age and physiological changes such as pregnancy can often be the cause. You should be able to manage the symptoms and even prevent them from occurring with the right guidance and lifestyle changes.
